兩公婆累鬥累|鼻鼾聲隨時係睡眠窒息症 免費網上講座問真啲兩公婆累鬥累|鼻鼾聲隨時係睡眠窒息症 免費網上講座問真啲
特約報道|睡覺扯鼻鼾看似是和伴侶及朋友閒談話題 - 有時我與太太討論到這個問題,她總喜歡先播放她手機中我的鼻鼾聲錄音。她坦言如果我在她熟睡後打鼻鼾不是問題,但我若比她先睡着,鼻鼾聲卻會讓她不能安眠。那麼對於打鼻鼾者又有甚麼影響?只不過製造一點噪音?還是有着更嚴重後果?
習慣性或原發性鼻鼾與睡眠呼吸障礙
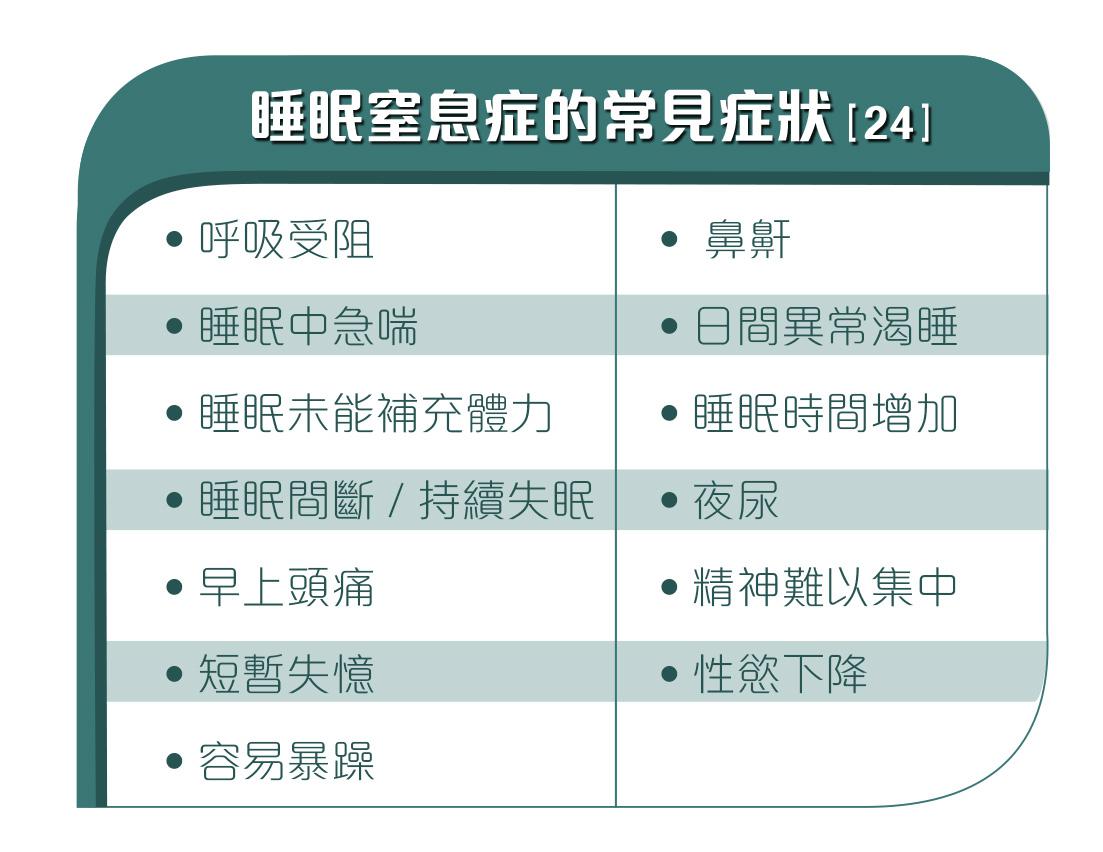
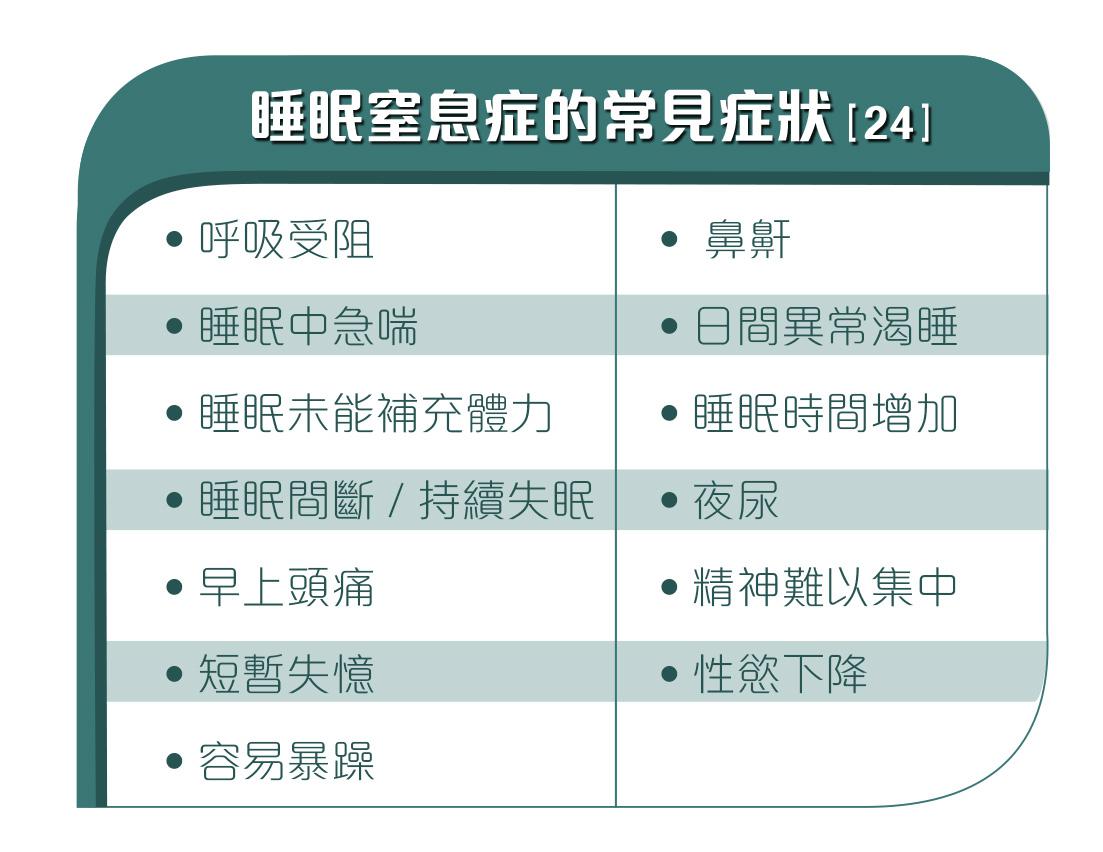
習慣性或原發性鼻鼾可能是睡眠呼吸障礙的主要症狀,可以是單一病症,亦可以和睡眠呼吸障礙的其他症狀同時出現。睡眠呼吸障礙其實包括從習慣性或原發性鼻鼾(簡稱PS)到睡眠窒息症(簡稱OSA)[1] 等一系列睡眠障礙。原發性鼻鼾是指睡夢中因上呼吸道震動而產生鼻鼾但沒有呼吸受阻 [2] 的症狀。睡眠窒息症指睡眠時呼吸重複受阻停頓,或因上呼吸道部份受阻,而持續超過10秒 [3]。睡眠窒息指數(簡稱AHI)以每小時出現呼吸受阻的次數劃分嚴重程度,指數高於5便可界定為睡眠窒息症 [4]。
為了進一步了解鼻鼾,澳洲在2006年進行了一項以人口為對象的縱貫性研究 [5],發現13%的成人在14年間出現習慣性鼻鼾。與習慣性鼻鼾相關的因素包括性別、肥胖、吸煙習慣,以及是否患上哮喘,另外一項在2011年進行的研究 [6]亦顯示鼻鼾與總死亡率上升有着重要關係。因此如果你有持續打鼻鼾,最好找醫生檢查一下。

睡眠窒息症令睡眠質素下降,讓患者難以集中精神,影響日常生活。

長期患上睡眠窒息症之後果
假如缺乏治療,長期患上睡眠窒息症有機會造成心臟病 [8] [9]、代謝紊亂 [10]、認知障礙 [11] 和抑鬱症[12]等。睡眠窒息症長期患者亦會出現生產力下降、涉及工業和交通意外而造成傷亡 [13] [14] [15]。長期患上睡眠窒息症可能產生嚴重後果 [16] [17],應該及時施以適當治療,才能紓緩病徵 [18] [19],減少出現後遺症 [20] [21]的機會。

研究顯示肥胖和睡眠呼吸障礙 [22] 息息相關,體重、年齡,都和睡眠窒息指數AHI有正向關係。瘦身減磅可減輕睡眠窒息症癥狀 [23]。
想知道如何初步評估自己有否患上睡眠窒息症?如何可以保持良好的睡眠質素?以至有關睡眠窒息症的種種問題?一直提供睡眠窒息症診療及治療方案的專家ResMed,將會舉辦「更好的睡眠。更好的表現 。」網上講座,內容包括:
1. 睡眠量Vs睡眠質量
2. 睡眠不足如何影響工作表現及引發慢性疾病
3. 睡眠窒息症分享過來人體驗
4. 睡得更好的秘訣
主持人阿Bob將會聯同香港中文大學醫學院呼吸系統科專科醫生吳素珊,一齊解答大家對睡眠窒息症的疑問,參加網上講座的人士更可獲得$100百佳現金禮券#。
#受有關條款及細則約束
網上講座詳情
日期:5月15日
時間:9:30am -10:45am
立即登記:https://bit.ly/3eVJRIm
1. Nisbet, L. C., Yiallourou, S. R., Walter, L. M., & Horne, R. S. (2014). Blood pressure regulation, autonomic control and sleep disordered breathing in children. Sleep Medicine Reviews, 18(2), 179-89. doi: 10.1016/j.smrv.2013.04.006
2. Zhu, Y., Au, C. T., Lam, H. S., Chan, C. C., Ho, C., Wing, Y. K., et al. (2014). Sleep architecture in school-aged children with primary snoring. Sleep Medicine Reviews, 15(3), 303-8. doi: 10.1016/j.sleep.2013.08.801
3. Malhotra, A., & White, D. P. (2002). Obstructive sleep apnoea. Lancet, 360(9328), 237-45. doi: 10.1016/S0140-6736(02)09464-3
4. Moon, K., Punjabi, N. M., & Aurora, R. N. (2015). Obstructive sleep apnea and type 2 diabetes in older adults. Clinics in Geriatric Medicine, 31(1), 139-47, ix. doi: 10.1016/j.cger.2014.08.023
5. Knuiman M, James A, Divitini M, Bartholomew H. Longitudinal study of risk factors for habitual snoring in a general adult population: the Busselton Health Study. Chest 2006; 130: 1779-1783.
6. Rich J, Raviv A, Raviv N, Brietzke SE. An epidemiologic study of snoring and all-cause mortality. Otolaryngol Head Neck Surg 2011; 145: 341-346.
7. Epstein LJ; Kristo D; Strollo PJ; Friedman N; Malhotra A; Patil SP; Ramar K; Rogers R; Schwab RJ; Weaver EM; Weinstein MD. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5(3):263–276.
8. 4. Kapur VK, Resnick HE, Gottlieb DJ, Sleep Heart Health Study Group Sleep disordered breathing and hypertension: does self-reported sleepiness modify the association? Sleep. 2008;31(8):1127–1132.
9. Walia HK, Li H, Rueschman M, et al. Association of severe obstructive sleep apnea and elevated blood pressure despite antihypertensive medication use. J Clin Sleep Med. 2014;10(8):835–843
10. Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569–576.
11. Olaithe M, Bucks RS, Hillman DR, Eastwood PR. Cognitive deficits in obstructive sleep apnea: insights from a meta-review and comparison with deficits observed in COPD, insomnia, and sleep deprivation. Sleep Med Rev. 2017 Mar;:30.
12. Wheaton AG, Perry GS, Chapman DP, Croft JB. Sleep disordered breathing and depression among U.S. adults: National Health and Nutrition Examination Survey, 2005–2008. Sleep. 2012;35(4):461–467
13. Mulgrew AT, Ryan CF, Fleetham JA, et al. The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med. 2007;9(1):42–53.
14. Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170(9):1014–1021.
15. Stoohs RA, Guilleminault C, Itoi A, Dement WC. Traffic accidents in commercial long-haul truck drivers: the influence of sleep-disordered breathing and obesity. Sleep. 1994;17(7):619–623.
16. Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep. 2006;29(3):299–305.
17. leep Health Foundation Asleep on the job: Costs of inadequate sleep in Australia. 2017:1–112.
18. Montserrat JM, Ferrer M, Hernandez L, et al. Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: a randomized controlled study with an optimized placebo. Am J Resp Crit Care Med. 2001;164(4):608–613.
19. Knudsen TB, Laulund AS, Ingerslev J, Homøe P, Pinholt EM. Improved apnea-hypopnea index and lowest oxygen saturation after maxillomandibular advancement with or without counterclockwise rotation in patients with obstructive sleep apnea: a meta-analysis. J Oral Maxillofac Surg. 2015;73(4):719–726.
20. George CF. Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal CPAP. Thorax. 2001;56(7):508–512
21. Dong Y, Dai Y, Wei G, Cha L, Li X. Effect of continuous positive airway pressure on blood pressure in hypertensive patients with coronary artery bypass grafting and obstructive sleep apnea. Int J Clin Exp Med.
22.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–3021.
24. Epstein LJ; Kristo D; Strollo PJ; Friedman N; Malhotra A; Patil SP; Ramar K; Rogers R; Schwab RJ; Weaver EM; Weinstein MD. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5(3):263–276. 2014;2014;7(11):4308–4315
-----------------------------
蘋果App大升級 更簡潔更就手!了解更多(立即下載體驗)
-----------------------------
蘋果初心不變!26周年「撐蘋果Tee」預售:
你的優惠訂購(海外訂購按此)